Sarah Houlton explains how the pharmaceutical industry finds new medicines
How the pharmaceutical industry finds new medicines
Where do new medicines come from? Modern medicine has come a long way from the herbs and other plants our ancestors relied on. Whether they are small molecule drugs or large biologics, such as genetically-engineered proteins, the medicines we take are almost all chemicals that have been invented by chemists.
The first medicines chemists designed were inspired by nature, particularly medicinal plants. Aspirin was derived from an extract of willow; belladonna came from deadly nightshade; opioid medicines such as morphine have their roots in the opium poppy. Medicines then started to be found in other natural materials, notably penicillin, which was isolated from a mould.
While nature has provided a rich source of ideas for medicines, there are many more diseases and conditions we want to treat for which no suitable natural compounds are available, or those we do find only have weak activity as medicines. Medicinal chemists now play a key role in the systematic design of the compounds that become pharmaceuticals.
Designing modern medicines
At the heart of modern medicine design is an understanding of the biochemistry of a biological effect, which allows molecules to be designed that either mimic the effect or stop it from happening. Most of the biological processes in our bodies that we want to disrupt chemically involve proteins, and so we want to create drugs that will interact with – and alter the behaviour of – the proteins associated with the disease we are trying to treat.
The first new medicine to be invented in this way, in the early 1960s, was the beta-blocker propranolol. It stops the activity of adrenaline at the beta-adrenergic receptors, and has a range of uses from lowering blood pressure to preventing migraines. Because it prevents the natural activity of the hormone adrenaline, it is called an antagonist.
At the heart of modern medicine design is an understanding of the biochemistry of a biological effect
One way to think about how this works is to imagine the beta-adrenergic receptor in the body as a lock and adrenaline as a key that fits and opens the lock perfectly. Propranolol, however, is a key that you can slide into the lock but it can’t be turned and unlocked. When a patient takes propranolol, it sits in the beta receptors and doesn’t activate them. Its presence blocks adrenaline from binding to the receptors, which is why it is called a beta-blocker.
Many other medicines have since been invented that work by blocking receptors like this. More still have been developed that are closer in design to the correct ‘key’ for a receptor, meaning they both fit in and ‘unlock’ the receptors. Drugs that can activate receptors like this are called agonists. A good example, which acts as an agonist at beta-adrenergic receptors, is the asthma medicine salbutamol.
In the early days of drug discovery, screening for medicinal activity was a laborious process. It involved taking individual molecules and seeing if they were able to kill bugs, or giving them to animals and looking for changes in behaviour. It was systematic, but slow, and far from sophisticated.
By the late 1980s, individual proteins could be isolated using the techniques of molecular biology. This allowed the ways molecules bind to proteins to be studied, and the strength of the binding interactions measured. Many measuring techniques were developed, most of which relied on adding fluorescent tags or radiolabels to the protein or the potential drug molecule, enabling them to be tracked.
Molecular starting points
The inspiration behind those early agonists and antagonists was the chemical structure of the natural hormone that fits into the target receptor. Its shape, and its functional groups, provide clues about the shape a drug molecule needs to be to fit into the receptor. Chemists could also design modifications to that natural structure that might alter its activity as required.
At first, this process was very much a case of trial and error. But over time so much knowledge has been built up about how different functional groups can affect activity at receptors that chemists are able to predict what changes they need to make to a molecule’s structure to achieve the response they are hoping for.
Chemists are now able to accurately modify the design of natural molecules to improve their affinity (how well they bind to the receptor), activity (how well they work) and selectivity (so they do not act at different receptors as well). The chemists will also do their best to tweak molecules to make them less likely to cause side-effects.
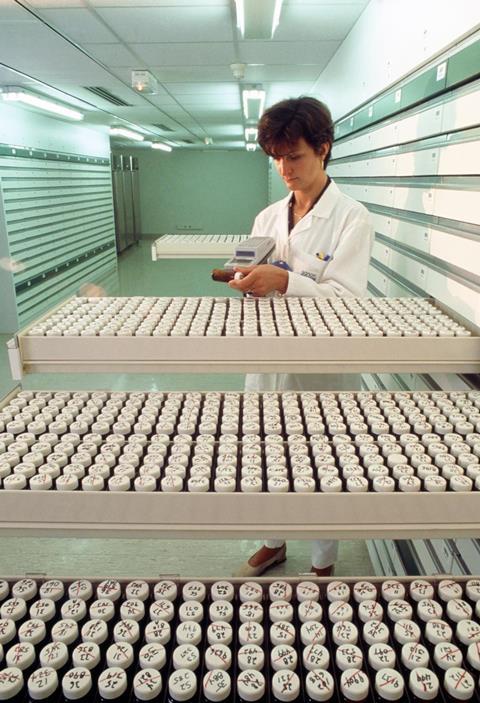
Nowadays, however, chemists don’t always use the natural hormone as their molecular starting point. Instead, the first ideas for new drug molecules often come from screening the target receptor against vast ‘libraries’ of different compounds. The purpose of these screens is to find ‘hits’ – molecules that have the desired activity in the receptor.
Because proteins are hugely varied in shape and structure, an equivalently varied collection of molecules is needed in these libraries. The libraries used by the pharmaceutical industry today contain millions of diverse molecules.
Automation has meant very tiny amounts of these vast numbers of compounds can be rapidly assessed, usually as mixtures of several compounds at once – a process known as high-throughput screening. The slow part in this process is developing the screen, known as a biological assay, which the molecules are going to be tested for activity against. This stage might take many months, but once it is done, screening a million compounds in a week is not unusual.
The next stage is working out the identity of individual hit molecules from the screening mixtures. This is a complex process that can be simplified if the individual molecules are tagged in some way that helps them to be identified. In DNA-encoded libraries, each building block is assigned a small sequence of DNA as an identifier.
Although DNA-encoded library technology is too new for any drugs it inspired to have reached the market yet, a handful are now in clinical trials. It has become a widespread tool, and many big pharma companies have invested heavily in the technology.
It is important to recognise that the molecules found via high-throughput screening are very unlikely to be suitable drugs in themselves. They will probably only have low affinity for the biological target, and they may not be sufficiently active. But they do provide that all-important starting point for medicinal chemists.
Going smaller
A high-throughput screening campaign will find molecules that interact reasonably strongly with the protein target in the screen, but they will often be fairly large, and contain several functional groups. However this isn’t always what chemists want as their molecular starting point.
Smaller molecules typically produce a weaker effect in the screens, which historically could be hard to detect. Improvements in analytical capabilities, particularly in x-ray crystallography and mass spectrometry, have now allowed much smaller interactions to be detected and measured, leading scientists to realise it might be possible to screen many fewer smaller but much weaker compounds.
This process is called fragment-based drug discovery. Rather than looking for molecules that already resemble drugs, like those molecules contained within a normal compound library, the idea is to use smaller, simpler ones that can be elaborated into more complex molecules later on by medicinal chemists. This may give a better insight into which functional groups could have a biological effect because there are fewer parts of the molecule that might be interacting with the target.
These fragments will typically have a molecular weight of about 150–200, have fewer than three hydrogen-bond donors or acceptors, and fewer than three bonds that can rotate. Because the interactions between the fragments and the biological target will be less strong than they are with a larger molecule, they also need to be very water soluble so that high concentrations can be screened.
Analytical techniques such as complex NMR experiments can be used, in addition to x-ray crystallography experiments, to study directly how these small fragments bind to the protein. This gives starting points for organic chemists to make more drug-like molecules, with better affinity to the target protein. It can also be possible to combine attributes from more than one fragment that binds in the same molecule.
Two anticancer drugs derived from fragment-based drug discovery have made it to the market – vemurafenib and venetoclax. Several more are undergoing clinical trials.
Phenotypic screens
Library techniques rely on making lots of molecules, and seeing whether they work in a screen designed to test them against a specific, known target. But in recent years, there has been something of a return to the old way of running a biological screen that looks for a physiological effect, and then working out which biological process was going on to cause that effect.
Instead of an isolated protein, the screen will use a cell, a tissue, or even a whole organism. This is known as phenotypic screening, because what is being measured is something to do with the function in the biology of that cell, tissue or organism. If it’s a screen for cancer or an infection, the biological effect is those cells multiplying, and the phenotype that we want to reverse is cell growth. Ideally, the molecule will kill the cells as it is cytotoxic, but it may simply arrest their growth, in which case it is cytostatic.
In more complicated biological systems, the cell’s function is studied. For example, in diabetes, you might take a pancreatic islet cell and look for molecules that alter glucose-stimulated insulin secretion. Or with an immune cell, you could be looking for molecules that affect the release of the proteins called cytokines that the cells use to communicate and signal action. For a neuronal cell, you might be looking at its electrical activity.
Once you have your hits, the next step is to work out what happens when these molecules are added to the cell, tissue or organism. Advances in techniques in chemical biology now allow us to look inside the cell and see how the molecules bind to proteins within. Today, multiple molecular processes can be observed and studied at the same time, whether they are taking place within cells, or on the surface of the cells.
Extremely sensitive mass spectrometry and fluorescence methods are the key to these advances, as they increasingly enable the detection of individual proteins among the thousands that are expressed by a cell.
Modern genetic techniques

The phenotypic screen is made more complex by the fact that, although you might be looking for one specific effect, however specialised its function is, a cell will always do many things other than that individual function. It can be hard to separate out the phenotype you are interested in from the normal business of living for the cell. It will also be dividing, respiring, and both making and consuming energy. These can interfere with the ability to see the effect that the screen is designed to observe.
To simplify this process, very targeted genetic modifications can now be used to edit the genome of the cells, and in so doing create biases that allow scientists to be confident what they are seeing in their screens is the effect they want to see, and not something else.
Gene editing can also be used to modify a binding site and see if it stops the original biological effect, or phenotype, from happening. Combinations of techniques from chemical biology and genetic engineering have sped up research that, in the past, would have taken many years, if not decades.
Modern DNA editing techniques, such as Talens and Crispr, are able to remove genes, insert genes, or replace genes with different ones in a very specific way. They exploit enzymes that have evolved to recognise particular DNA sequences within the genes using small fragments of DNA as guides. Those guides can be synthesised, and are the means by which the gene editing is done in a directed and targeted way. These techniques have the potential to help us understand the complexity of DNA sequence variation and, ultimately, improve target identification for new medicines.
Sarah Houlton is a science writer based in Boston, US
Suggested teaching resources
- Masterminding molecules: An interactive game where you answer brain-teasing questions and learn what is involved in making a medicine. Progress through three levels and determine which shapes, structures, properties and interactions between molecules make the best medicines.
- Which compound? Which route? This exercise leads students through the decision-making process when choosing which new drug substance to make and the best synthetic route.










No comments yet